A cataract is a gradual clouding of the eye’s natural lens the clear structure behind the colored iris that helps focus light onto the retina. When the lens loses its transparency, light scatters instead of forming a crisp image, and vision can become blurred, dim, or glary. Cataracts are common with aging, but they can also develop earlier due to health conditions, medications, injury, or prolonged sun exposure. Because the change is often slow, many people adapt without realizing how much clarity they’ve lost until daily tasks feel harder than they should.
How a cataract develops inside the eye
The lens is made of water and proteins arranged in a very orderly way to keep it clear. Over time, those proteins can break down and clump together, creating cloudy patches that interfere with the path of light. The location of the cloudiness matters: some cataracts start in the center, while others form more toward the edges or the back of the lens, and each pattern can affect vision in slightly different ways. Although cataracts are not usually painful, their steady progression can interfere with independence, especially when driving, reading, or working on screens becomes uncomfortable.

Why clarity and contrast drop first
One of the earliest functional changes is reduced contrast sensitivity. Even if you can still read an eye chart reasonably well, subtle details may seem harder to distinguish like gray text on a white background or steps and curbs in low light. This happens because a cloudy lens diffuses light, which washes out fine edges and makes objects blend together. Many people interpret this as “tired eyes,” but it’s often the first clue that the lens is no longer delivering a clean, focused image to the retina.
The most common ways cataracts affect vision
Cataracts can show up differently from person to person, but several symptoms are especially common. Changes often appear in real-life lighting rather than in perfect indoor conditions, so it helps to notice patterns in your daily routine.
Vision changes people describe most often
- Blurry or “filmy” vision that doesn’t improve even after cleaning glasses
- Increased glare from sunlight, lamps, or oncoming headlights
- Halos or starbursts around bright lights at night
- Colors looking faded, yellowed, or less vibrant than before
- Needing brighter light to read comfortably
- Frequent changes to glasses or contact lens prescriptions that still feel “off”
When these issues start interfering with daily life, many people begin researching treatment options and comparing expertise, including looking for the best cataract surgeon in vadodara to understand what modern care can achieve and what outcomes are realistic.
Understanding glare, halos, and night-driving difficulty
Night driving becomes challenging because the pupil widens in dim conditions to let in more light. If the lens has cloudy areas, that extra incoming light is scattered rather than focused, creating glare and halos. Headlights can feel painfully bright, and it can take longer to recover after looking at a strong light source. Wet roads, reflective signs, and high-beam traffic intensify the problem, which is why some people avoid driving after dusk even before they feel significantly “blind” during the day.
Simple adjustments that may help temporarily
- Use anti-reflective coatings on glasses to reduce scattered light
- Keep windshields and eyeglasses extremely clean to minimize additional glare
- Increase ambient lighting at home for reading and cooking
- Reduce night driving when possible until you’re evaluated
These measures may improve comfort, but they don’t remove the clouding in the lens.
Different cataract patterns and what they tend to cause
Cataracts are often categorized by where the clouding occurs in the lens. Knowing the general type can help explain why your symptoms feel more like glare issues, reading difficulty, or overall blur.
Common patterns clinicians may identify
- Nuclear changes (center of the lens): gradual yellowing and reduced distance clarity
- Cortical changes (outer layers): streaks that increase glare and reduce contrast
- Posterior subcapsular changes (back of the lens): stronger glare in bright light and difficulty reading or using screens
An eye exam can determine which pattern is present and whether other eye conditions are contributing to your symptoms.
Who is more vulnerable and why it matters
Age is the leading risk factor, but several other influences can speed up lens clouding. Understanding risk helps you take protective steps and recognize when it’s time to get checked rather than waiting years.
Factors associated with faster cataract development
- Long-term UV exposure without sunglasses or a hat
- Smoking and heavy alcohol use
- Diabetes and poor blood sugar control
- Long-term steroid medication use (including some eye drops)
- Prior eye injuries, inflammation, or surgery
- Family history of cataracts
Reducing UV exposure, managing chronic health conditions, and stopping smoking can support overall eye health, even if they can’t guarantee prevention.
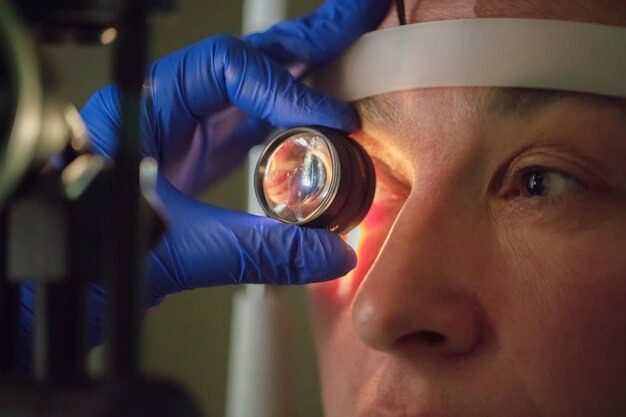
When symptoms are worth checking promptly
Because cataracts progress gradually, it’s easy to delay an evaluation. However, certain changes should trigger a timely appointment, particularly if they affect safety or daily functioning. During an exam, clinicians assess visual acuity, glare sensitivity, and the lens under magnification, and they also look for retinal or optic nerve issues that can mimic cataract symptoms.
Clues that an exam shouldn’t wait
- Vision that suddenly feels much worse in specific lighting conditions
- Glare that makes driving feel unsafe
- Reading fatigue that doesn’t improve with stronger lighting
- One eye seeing much more poorly than the other
If you notice early signs of cataracts, an exam can confirm whether lens clouding is the cause or whether another treatable condition like dry eye or refractive error is driving the problem.
What treatment looks like at different stages
In mild cases, updating a prescription, improving lighting, and using anti-glare lenses may help you function comfortably for a while. But once clouding progresses enough to interfere with quality of life, surgery becomes the definitive option. Cataract surgery replaces the cloudy natural lens with a clear artificial lens implant, aiming to restore clarity and reduce glare an approach that also reflects what’s next in surgery as techniques and lens technologies continue to evolve for more personalized visual outcomes.
What people often ask before deciding
- Whether both eyes need treatment and how timing is planned
- Which lens implant options fit their lifestyle (reading, screens, driving)
- What recovery typically feels like and how quickly vision stabilizes
- How to balance cost, convenience, and surgeon experience
At this stage, it’s common for patients to seek consultations and compare experience and technology, and some will prioritize finding the best cataract surgeon in vadodara based on outcomes, communication style, and comfort with the recommended approach.
Making informed choices for better vision
Choosing when to treat a cataract is often less about a single test result and more about how vision changes affect your real-world life. A thorough evaluation clarifies what portion of blur is from lens clouding versus other causes, and it sets expectations for what improvement is likely after treatment. As symptoms increase, it helps to keep a short log of situations that feel difficult night driving, reading labels, or seeing faces in dim rooms so you can describe functional limitations clearly during your visit. When you’re ready to move forward, discussing options with a trusted specialist, including the best cataract surgeon in vadodara, can make the process feel structured, predictable, and aligned with your goals.
Conclusion
A cataract is a clouding of the eye’s natural lens that scatters light and gradually reduces clarity, contrast, and comfort often showing up first as glare, halos, and difficulty in low light. While early adjustments like brighter lighting and updated prescriptions may help for a time, cataracts typically progress and can eventually interfere with safety and daily independence. The most important step is getting an eye evaluation when vision changes begin to limit your routine, so you can confirm the cause and discuss the right timing and options for restoring clear sight.